Diagnostic methods for the detection of acute gastroenteritis
Acute gastroenteritis is among the most common causes of morbidity and mortality worldwide1, with the highest prevalence observed in non-industrialised countries as the disease is most frequently transmitted under conditions of poor hygiene or by consuming contaminated food or water.2 However, acute gastroenteritis remains a common condition in both low- and high-income countries.3 Symptoms and complications have led to a significant impact on workload and economic burden for the healthcare system and society.3 For example, in the Netherlands and Belgium, annual direct medical expenditure due to acute gastroenteritis amounts to 945 million euros and 112 million euros, respectively.3,4 Similarly, in Finland, the loss of efficiency and the associated cost of lost work days were estimated at 1.8-2.1 million euros, with the prevalence of workers absent due to illness recorded at 3.54 times higher in the week following an outbreak.5
Acute gastroenteritis is responsible for 1.45 million deaths worldwide

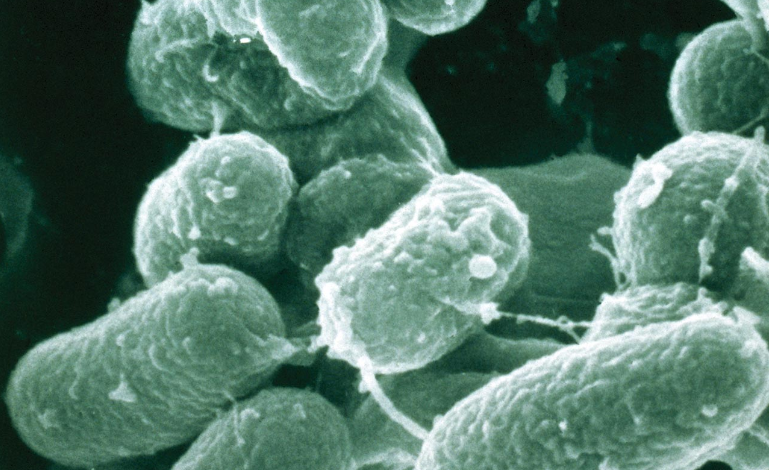
Gastroenteritis is a transient disease that can be caused by a multitude of different viral, bacterial, and parasitic pathogens.6 Norovirus is the pathogen most commonly responsible for acute gastroenteritis in the United States, followed by Salmonella spp., Shigella spp. and Shiga toxin-producing E-coli (STEC). Among children in particular, Rotavirus is the pathogen of greatest clinical relevance7. It is estimated that, in 2013, Rotavirus was responsible for the deaths of more than 200,000 children worldwide, and the most recent estimates of mortality from this virus range from 500 to 600 deaths per day.7
Improvements in sanitation have led to an overall reduction in bacterial and parasitic infections.1 However, increases in hospital admissions related to diarrhoea attributed to acute viral gastroenteritis have reached alarming levels, with at least one viral agent in nearly 43% of childhood diarrhoea samples in developing countries.8 In any case, even in high-income countries, economic development is creating opportunities for the introduction and transmission of enteric pathogens, posing a serious health problem.9
Rapid testing is essential
Because infants and the elderly are particularly susceptible to complications stemming from acute gastroenteritis, rapid targeted testing helps guide practitioners towards the appropriate type of treatment for patients in intensive care.10 In addition, given the highly infectious nature of the disease, hospitals are in short supply of isolation facilities.11
Rapid testing for gastrointestinal infections can, for some patients, reduce the time spent in isolation, or otherwise reduce the time spent waiting for suitable treatment, thereby minimising the overall burden involved. Several diagnostic techniques are currently in use with the aim of improving patient management and avoiding life-threatening consequences of acute gastroenteritis. In the next section, we will explore these and highlight their main advantages.
Acute gastroenteritis is responsible for 1.45 million deaths worldwide

The conventional diagnosis of enteric gastrointestinal infections is based on three main techniques: microscopic examination (parasites), cultures on plates combined with antimicrobial susceptibility testing (AST), and antigen detection using immunological tests.1,2 These methods involve several steps and procedures, which means that results may take up to 3 to 5 days to become available. For vulnerable patients, such as infants, health can deteriorate rapidly when suffering from an infection, so when time is a determining factor for survival, the speed of a diagnostic technique is imperative. Each diagnostic technique has its advantages and disadvantages in the clinical setting.
Use of stool cultures for the diagnosis of acute gastroenteritis
Enteric bacteria are responsible for more severe cases of infectious diarrhoea than other infectious etiologies, and one study found a bacterial origin in 87 percent of cases.12 Routine co-cultures (stool cultures) that can identify common bacteria are normally required in the first instance: Salmonella, Campylobacter, and Shigella.12 However, there are some microorganisms that cannot be easily cultured in the laboratory, or that require specific conditions which, if not met, can result in failure or significant delay in detecting the pathogen. Another major problem concerns the length of time taken to obtain the diagnostic result. For example, the detection of Shigella by culture is possible but should be avoided in primary diagnosis because of the long response time, up to 5 days.2,13 Samples require a long incubation time , and the sensitivity of the result is affected by a number of factors, including the type and quality of the sample, the patient’s age, appropriate transport, and the culture medium.2
The ability of plate cultures to identify pathogens has been evaluated over the years. One study compared pathogen detection using conventional methods, including culture, with multiplex real time PCR on 182 patients with diarrhoea. The study found that significantly more pathogens were detected using the multiplex panel (58.3%) than in the conventional studies on faeces (42.3%), and the average time taken to report was reduced from 25 hours after the hospital consultation to 4 hours.14 In each case, the time taken to report was significantly shorter than that of the conventional methods, which took an average of 72 hours.14
Considering these data and the extensive adoption of molecular platforms in laboratories during the COVID-19 emergency, should we expect molecular diagnostic tests to become a popular type of testing for infectious gastroenteritis as well?
The answer may be yes. However – as discussed in the article previously published in BD Academy, on the detection of hospital infections and antibiotic-resistant organisms15 (go to article) and clearly highlighted in the recently updated AMCLI Diagnostic Pathway flowchart9 – it is important to consider molecular diagnostics not as a substitute, but as a complement to conventional methods in the laboratory workflow. In fact, since when diagnosing infectious gastroenteritis most specimens test negative if a stool culture is used as the primary test9, to maximise efficiency in the laboratory and the speed of obtaining a result for practitioners (within 4 hours), molecular methods could themselves be used as a primary test for the initial screening of samples.
This would enable practitioners to promptly refer negative patients for the investigation of other noninfectious causes of diarrhoea, and enable the laboratory to focus its attention and efforts on phenotypic confirmation/isolation of the microorganism/detailed analysis of antibiotic resistance using plate cultures performed only on samples that tested positive in the molecular testing. The isolation of the microorganism and further phenotypic characterisation are, in fact, also of great relevance in nationally/internationally managed supervision and the planning of possible activities related to public health protection9.
Advances in molecular diagnostics are making the targeted diagnosis of acute gastroenteritis possible
Commercially available molecular tests have changed the way the laboratory diagnosis of enteric infections is performed.2 Molecular tests have been shown to be more sensitive and specific than traditional methods and, in the case of acute gastroenteritis, the disease can be diagnosed earlier in the course of the infection, even when the level of microbial load is low.1 NAATs identify the pathogen in question regardless of culture constraints and demonstrate good inter-laboratory reproducibility.16
Although the cost of reagents and instruments used in real time PCR technology are greater than in conventional techniques such as co-culture, the level of automation provided significantly reduces operator time and turnaround time (TAT).2 The efficiency of automation makes the molecular method much less labour intensive and more standardised than conventional techniques.
Multiplex PCR-based tests simultaneously analyse stool samples for the presence of a number of pathogens. Extended multiplex panels (which can even detect vast numbers of pathogens in the same reaction) run the risk of producing false positive results in the case of rare pathogens.17 Moreover, it is important that the platform running the tests is integrated and does not require the extraction of nucleic acids to be performed separately from the amplification and detection of targets, to minimise cross-contamination and false positive results in subsequent runs.2 When these criteria are met, a targeted approach (i.e., targeted testing for clinically relevant key pathogens based on patient history performed by the practitioner) can be used to test various pathogens known to cause the same syndrome in patients. Integrated platforms have a substantial impact on management, with the potential to reduce the time taken for initial identification of a pathogen, affect the outcome for patients through early initiation of targeted antibiotic therapy, improve antimicrobial management and, ultimately, optimise infection control.18
Example of cost-benefit analysis of targeted molecular enteric panels
Ferrer et al. conducted a cost-benefit analysis of health care system spending on the diagnosis of acute infectious gastroenteritis using the BD MAX™ Enteric Bacterial Panel, the BD MAX™ Extended Enteric Bacterial Panel and the BD MAX™ Enteric Viral Panel.19 The researchers used a Markov model on 1,336 retrospectively clinically reviewed medical records to track the probability of transition between different health conditions, from the time when the faeces were analysed to the completion of treatment related to gastroenteritis during two 6-month periods in which both conventional procedures and BD MAX™ PCR multiplex panels were used.19
From this model, they found that the total cost of health care for an individual with acute gastroenteritis was 341 euros in the case of conventional procedures and 314 euros when using PCR, while the costs for a pediatric patient were 456 and 271 euros respectively.19
The authors showed that the use of BD MAX™ Enteric Panels, when compared with conventional non-PCR-based approaches, resulted in an incremental cost benefit.5 Specifically, with the implementation of molecular testing, they reported a saving of €27 per patient.5 The saving rose steeply to €185 per patient when only paediatric patients were considered.19 These savings can be attributed to the reduced demand on health care services and more judicious use of antibiotics.19
Ferrer et al. concluded that multiplex molecular panels, such as those studied on the BD MAX™ system, enable the rapid, sensitive and accurate diagnosis of acute infectious gastroenteritis on the part of laboratories, which can lead to quicker therapeutic decisions and infection control measures.19
Monitoring of Enteric Pathogens in Italy
As with the monitoring of hospital infections, the newly published PNCAR 22-25 emphasises the importance of monitoring enteric pathogens as well20. In Italy, the Enter-Net (Enteric Pathogen Network) laboratory monitoring network, coordinated by the Department of Infectious Diseases of the Italian National Institute of Health, collects epidemiological and microbiological information relating to the isolation of Salmonella, Campylobacter, Shigella, Yersinia, Vibrio and other enteric pathogens of human origin. Among the specific goals of the Enter-Net network are20:
– to obtain descriptive data on enteric pathogens isolated from human cases, including phenotypic characteristics of isolated strains through standardised protocols;
– to identify national and international epidemic events and, where required, collaborate with relevant health authorities by providing epidemiological and laboratory support and liaison between the various national and international institutions involved.
BD solutions for the diagnosis of infectious gastroenteritis
BD offers a wide range of solutions that can be used throughout the laboratory diagnostic pathway for infectious gastroenteritis, in line with the needs of the microbiology laboratory.
In particular:
– the range of targeted, validated molecular panels for the fully automated BD MAX™ system ensures prompt, accurate detection of enteric bacteria/viruses/parasites which, if combined with appropriate antimicrobial treatment, can prevent transmission and improve patient management. Find out more about molecular tests available for the detection of enteric pathogens (with great flexibility in the analysis of clinically relevant bacteria). The available tests have now been validated on both fresh faeces and samples collected using the FecalSwab™.
– solutions for culture and phenotypic analysis (manual and automated), including the BD Phoenix™ M50 system and respective panels, combined with the BD Bruker MALDI BioTyper® and BD Epicenter™middlware, which provides accurate ID/AST results for the correct classification of the microorganism and the prescription of antibiotics.
BD-115567
Bibliography
1. Sidoti F, Rittà M, Costa C, et al. Diagnosis of viral gastroenteritis : limits and potential of currently available procedures. J Infect Dev Ctries 2015;9:551-561.
2. Amjad M. An Overview of the Molecular Methods in the Diagnosis of Gastrointestinal Infectious Diseases. Int J Microbiol 2020;2020:1-13. Available at: https://www.hindawi.com/journals/ijmicro/2020/8135724/.
3. Papadopoulos T, Klamer S, Jacquinet S, et al. The health and economic impact of acute gastroenteritis in Belgium, 2010–2014. Epidemiol Infect 2019;147:e146. Available at: https://www.cambridge.org/core/product/identifier/S095026881900044X/type/journal_article.
4. Pijnacker R, Mangen M-JJ, van den Bunt G, et al. Incidence and economic burden of community-acquired gastroenteritis in the Netherlands: Does having children in the household make a difference? Riddle MS, ed. PLoS One 2019;14:e0217347. Available at: https://dx.plos.org/10.1371/journal.pone.0217347.
5. Halonen JI, Kivimäki M, Oksanen T, et al. Waterborne Outbreak of Gastroenteritis: Effects on Sick Leaves and Cost of Lost Workdays. Nizami Q, ed. PLoS One 2012;7:e33307. Available at: https://dx.plos.org/10.1371/journal.pone.0033307.
6. NICE. Gastroenteritis : Summary. NICE 2020. Available at: https://cks.nice.org.uk/topics/gastroenteritis/. Accessed October 1, 2021.
7. Epicenter-ISS site. https://www.epicentro.iss.it/rotavirus/epidemiologia . Visited 2 December 2022.
8. Ramani S, Kang G. Viruses causing childhood diarrhoea in the developing world. 2009:477-482.
9. AMCLI ETS. Percorso Diagnostico “Enteriti di Origine Infettiva” – Rif. 2023-07, rev. 2023″ https://www.amcli.it/wp-content/uploads/2023/05/07_PD-enteriti-di-origine-infettiva_def25mag2023-2.pdf
10. Freeman K, Mistry H, Tsertsvadze A, et al. Multiplex tests to identify gastrointestinal bacteria, viruses and parasites in people with suspected infectious gastroenteritis: a systematic review and economic analysis. Health Technol Assess (Rockv) 2017;21:1-188. Available at: https://www.journalslibrary.nihr.ac.uk/hta/hta21230.
11. Sandmann FG, Jit M, Robotham JV, et al. Burden, duration and costs of hospital bed closures due to acute gastroenteritis in England per winter, 2010/11–2015/16. J Hosp Infect 2017;97:79-85. Available at: https://linkinghub.elsevier.com/retrieve/pii/S0195670117302852.
12. Sattar SBA, Singh S. Bacterial Gastroenteritis.; 2021. Available at: http://www.ncbi.nlm.nih.gov/pubmed/30020667.
13. Moro DD, David MO. Infectious Gastroenteritis: Causes, Diagnosis, Treatment and Prevention. Lupine 2019;2:1-6.
14. Yoo IH, Kang HM, Suh W, et al. Quality Improvements in Management of Children with Acute Diarrhea Using a Multiplex-PCR-Based Gastrointestinal Pathogen Panel. Diagnostics 2021;11:1175. Available at: https://doi.org/10.3390/diagnostics11071175.
15. BD Academy NEWS. Le tecniche di screening molecolare per organismi multiresistenti ai farmaci (MDRO) possono ridurre i tassi di mortalità e l’onere economico della resistenza antimicrobica (AMR). https://bdacademy.bd.com/le-tecniche-di-screening-molecolare-per-organismi-multiresistenti/ Novembre 2022.
16. Rodger AG, Morris-jones S, Huggett J, et al. The role of nucleic acid amplification techniques ( NAATs ) in the diagnosis of infective endocarditis. Br J Cardiol 2010;2010:195-200.
17. Pankhurst L, Macfarlane-Smith L, Buchanan J, et al. Can rapid integrated polymerase chain reaction-based diagnostics for gastrointestinal pathogens improve routine hospital infection control practice? A diagnostic study. Health Technol Assess (Rockv) 2014;18:1-167. Available at: https://www.journalslibrary.nihr.ac.uk/hta/hta18530/.
18. Chang L-J, Hsiao C-J, Chen B, et al. Accuracy and comparison of two rapid multiplex PCR tests for gastroenteritis pathogens: a systematic review and meta-analysis. BMJ Open Gastroenterol 2021;8:e000553. Available at: https://bmjopengastro.bmj.com/lookup/doi/10.1136/bmjgast-2020-000553.
19. Ferrer J, Giménez E, Carretero D, Buesa J, Morillas F, Granell R, Fuenmayor A, Navarro D, Albert E. BD MAX Enteric Bacterial, Bacterial Plus, and Virus Panels for Diagnosis of Acute Infectious Gastroenteritis: a Cost-Benefit Analysis. Microbiol Spectr. 2022 Oct 26;10(5):e0088022. doi: 10.1128/spectrum.00880-22. Epub 2022 Sep 7.
20. Redazione Aboutpharma. Antibioticoresistenza: il nuovo Piano nazionale 2022-25 è all’esame delle Regioni. 21 September 2022. https://www.aboutpharma.com/animal-health/antibioticoresistenza-il-nuovo-piano-nazionale-2022-25-e-allesame-delle-regioni/

 It is estimated that over the next 35 years MDR-TB will cost the global economy $16.7 trillion.5 If current trends continue, MDR-TB could kill an estimated 75 million people worldwide by 2050.5 If not kept under control, models have estimated that over time the proportion of drug-resistant tuberculosis will continue to increase and become more difficult and more expensive to treat.5
It is estimated that over the next 35 years MDR-TB will cost the global economy $16.7 trillion.5 If current trends continue, MDR-TB could kill an estimated 75 million people worldwide by 2050.5 If not kept under control, models have estimated that over time the proportion of drug-resistant tuberculosis will continue to increase and become more difficult and more expensive to treat.5